Reviewed by Gabrielle Fundaro, PhD, CISSN, CHC
“I can’t go out tonight, I’m… busy.”
If you struggle with gut health problems, you know this line is often code for one—or all—of the following:
“I have to stay close to the bathroom.”
“I can’t wear real pants right now.”
“My farts might kill you.”
Digestive symptoms like gas, bloating, indigestion, and toilet troubles are common—and can be extremely disruptive (and not just to your social life).
But if you’re frequently plagued by these issues, all you really want to know is:
What will actually help my belly feel better??!
A lot, actually.
In the following story, you’ll discover:
- How stress, exercise, and many other factors affect your gut health and microbiome
- How to restore gut health after taking antibiotics
- Whether you’re the kind of person who could benefit from extra fiber
- If fermented foods live up to their hype
- Which supplements might help symptoms like constipation, heartburn, and more, according to research
Most important, you’ll find five evidence-based, cost-effective ways to improve gut and microbiome health overall.
First, what the heck is the microbiome?
This community of microorganisms (bacteria, fungi, and and their genetic material) lives on your skin, in your mouth, in your lungs, and throughout your digestive tract.
Researchers estimate that between 10–100 trillion microorganisms live in your GI tract alone.
Which means: Your body is basically a human-shaped pile of bacteria.
Your microbiome is as unique as your fingerprint.
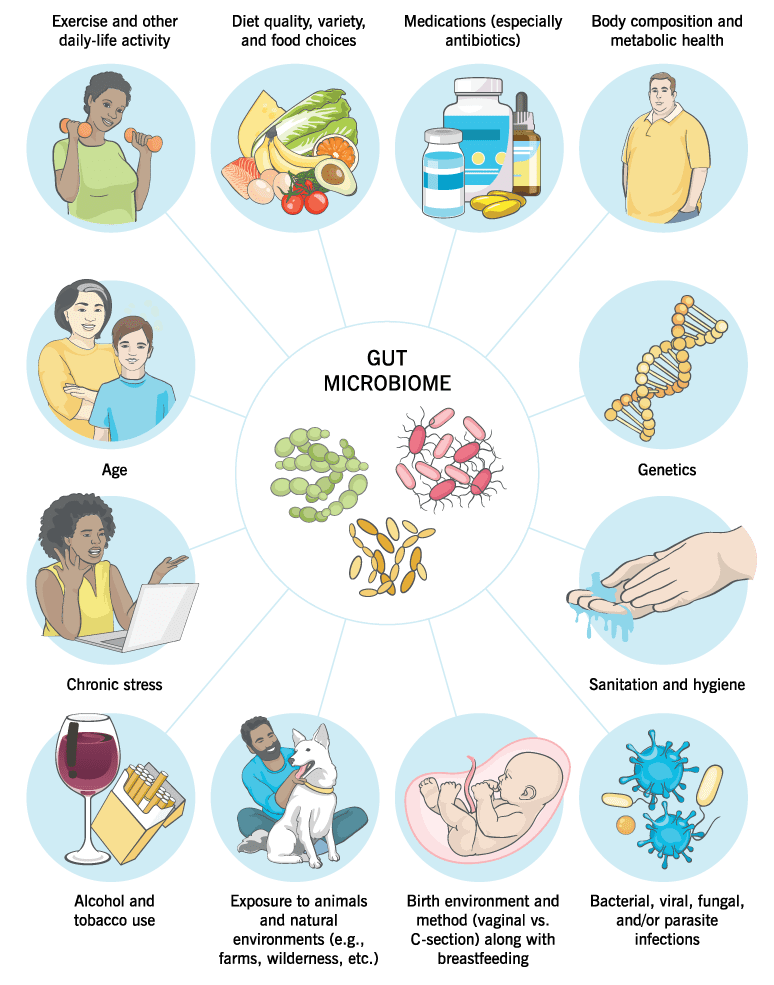
The amount and proportions (aka. diversity) of bacteria and fungi will also change throughout your life, depending on a variety of influences, as the image below shows.
Many of these critters are like barnacles on a whale. They hitch along for the ride at no cost to you.
Many others are beneficial, helping to keep your skin, gums, and GI tract healthy. These friendly gut bacteria help:
- Produce small amounts of nutrients, like vitamins B and K
- Ferment fiber and resistant starch which create short-chain fatty acids (SCFAs) that help regulate your immune system, appetite, and stress response1 2
- Keep the system moving (a.k.a. pooping regularly) by bulking up stool and increasing gut motility
- Regulate inflammation and the immune system
Though there’s still a lot researchers don’t know about the microbiome, they do know this:
Your gut bacteria play a major role in your health and wellbeing.
With that in mind, here are five practical, science-based strategies to support these beneficial, hard-working little friends—and in turn, promote good digestive function, and overall health.
How to support gut health
These strategies can help you improve bacterial diversity and digestive function, as well as reduce the risk of disease.
1. Chew your food.
When you slowly and thoroughly chew food, you break your meal down into smaller, more digestible bits. The smaller pieces also increase the amount of surface area for digestive enzymes to work on and aid chemical digestion.
On the other hand, when you eat quickly, you tend to gulp down big chunks of food—and likely lots of air—which can lead to indigestion and bloating. Plus, those enzymes have a harder time digesting larger pieces of food.
If possible, give yourself a little extra time at meals.
Pay attention to your food (at least intermittently), pause to breathe every once in a while, and put your teeth to work, aiming for the texture of applesauce before each gulp.
2. Include many different types of minimally-processed plant-based foods.
Fruits, vegetables, whole grains, starchy tubers, beans, and other minimally-processed plant foods do two handy things for your gut:
- They feed gut bacteria. When bacteria chows down on fiber, it multiplies and contributes to short-chain fatty acid production as well as bacterial diversity.
- They provide bacteria with helpful phytochemicals (like polyphenols) that can be transformed into antioxidant and antiinflammatory compounds.3 4
(Want help choosing minimally-processed foods? Check out: ‘What should I eat?!’ Our 3-step guide for choosing the best foods for your body)
Meanwhile, if you eat mostly highly-processed foods (and not a lot of minimally-processed foods) the diversity and activity of your microbiome reduces.5
In rat studies, this has been shown to skew the overall environment toward bacteria that may increase inflammation and disease risk, hunger and appetite, and vulnerability to the effects of stress, like mood or hormonal imbalances.6
(To be clear, we’re not suggesting you cut processed foods out altogether. In the context of a healthy diet, indulging might actually be good for you. See: How to eat junk food: A guide for conflicted humans.)
Are fermented foods good for the gut?
Kombucha. Natto. Sauerkraut. Kimchi. Yogurt.
About a decade ago, food and beverage products with “live bacterial cultures”—and claims to improve digestion—exploded onto the market.
(Of course, many of these foods have existed for centuries as food staples in certain cultures. As many Eastern Europeans will tell you: “Kvass is old news!”)
But do they work?
We’ll cut to the chase:
Only fermented dairy (specifically, kefir) is supported by high-quality evidence. Even then, its benefits seem to apply more to cardiometabolic health than to digestive health.7
A recent study that’s gotten a lot of buzz implies that a range of other fermented foods may increase microbiome diversity, but more research is needed to determine whether this is due to the ferments themselves or simply the inclusion of new minimally-processed foods.
So, while lacto-fermented veggies and sourdough are delicious and can contribute to a varied, nutrient-dense diet, there’s no guarantee (and no indisputable evidence, to date) they’ll improve your digestion or elimination.
3. Add a fiber supplement. (Maybe.)
This might come as a shock:
Not everyone benefits from more fiber.
[Flings cardboard-like high-fiber cereal into the fire]
If you consume a diet rich in minimally-processed foods, your diet is already naturally rich in fiber. And adding even more of the stuff may not move the digestive needle much, if at all.
On top of that, some people are sensitive to compounds called FODMAPs—which stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols—found in specific fiber-rich foods. When they eat these foods, they’ll experience gas, bloating, and loose stools.
The above caveats aside, there are a few scenarios where a fiber supplement can be a good idea:
▶ You struggle to eat minimally-processed foods.
This might be because you can’t readily access them, or because you can’t tolerate the taste.
Consider supplementing with a mix of soluble and insoluble fiber. Also, experiment with adding whole foods like fruits, vegetables, whole grains, and legumes for more fiber and an overall nutrition boost.
▶ You eat mostly minimally-processed foods, but you avoid carbs.
In other words, you mostly eat non-starchy vegetables, animal proteins, and healthy fats.
If your gut functions well, you likely don’t need to make any changes.
However, if your poops are infrequent, hard to pass, or very small, consider adding more soluble fiber, either through foods like beans, lentils, oats, or sweet potatoes (if you’re willing to alter your macro split), or through a supplement like psyllium powder.
(For TMI on exactly what an ideal poop should look like, check out: Are your eating and lifestyle habits REALLY working? Just ask your poo)
▶ Despite eating a full range of minimally-processed foods, you still struggle with constipation.
Although psyllium (a soluble fiber) might help with constipation, it can actually worsen other problems like diarrhea, gas, and bloating. Before adding it, talk to your doctor or healthcare practitioner to rule out food allergies, intolerances, or other causes of digestive distress.
(An elimination diet can be a great way to assess if you’re reacting negatively to certain foods. Here’s a primer to get you started: Elimination diets: How and why to do them.)
Crash course: Soluble vs. Insoluble Fiber
If you’re interested in changing your fiber intake (maybe because you’ve heard it might help a digestive issue) it can help to know the difference between the two types of fiber.
▶ Soluble fiber absorbs water. This creates a gel that softens stool. Soluble fiber also feeds beneficial gut bacteria.8
Foods like whole grains, beans, legumes, and psyllium are rich in soluble fiber.
▶ Insoluble fiber doesn’t dissolve in water. It adds bulk or weight to stool, making it easier and often faster to pass. Because it helps improve bathroom regularity, insoluble fiber reduces the risk of GI symptoms9 and bowel diseases.10
Many non-starchy vegetables and wheat bran are good sources of insoluble fiber.
Note: If you’re currently eating a very low fiber diet and start incorporating more fiber—either through whole foods or supplements—sometimes there’s an adjustment period.
For a couple of weeks, you might notice extra gurgling, gas, and maybe changes in bowel activity. If it becomes too uncomfortable, scale back for a period of time. Reintroduce more moderately when you’re ready.
Eventually, most people adjust and find their appetite, digestion, and overall health greatly benefit from adequate fiber.
4. If you have to take antibiotics, add some good bacteria back in.
Antibiotics can be life-saving. And at some point, almost all of us will have to take them.
(Note: Only a doctor can decide when antibiotics are—or aren’t—appropriate.)
However, antibiotics are associated with less microbial diversity in the gut, as well as an increase of “bad” bacteria (think: C. difficile, Salmonella, and antibiotic-resistant Enterococcus).11
In healthy people, gut bacteria levels recover pretty well—but not perfectly—after taking antibiotics.
In one study, people recovered to close to their pre-antibiotic baseline within six weeks, but were still missing several strains of bacteria that had been present before the antibiotics six months later.12
In some cases, probiotics—supplemental beneficial bacteria—can help.
Especially in the case of antibiotic-associated diarrhea, supplements containing Lactobacillus rhamnosus GG and Saccharomyces boulardii seem to work well to prevent symptoms.13
Just bear in mind not everyone responds to specific probiotics in the same way.
Individual response depends on the bacteria you already have in your gut, plus whether the supplemental bacteria takes up residence in your GI tract or just passes through.
(To find out when probiotics are most useful, read: Do probiotics really work?)
5. Move.
Physical activity and cardiovascular fitness are associated with more microbial diversity and more short-chain fatty acids.14 15 16
(Recall: SCFAs do lots of good things for the body, from better immunity, to better tolerance to stress.)
Additionally, when you engage in mild-moderate exercise, you stimulate the parasympathetic (“rest and digest”) nervous system.
Not only does this have an overall relaxing effect on the body and mind, but it also encourages movement (peristalsis) in the digestive tract, aiding both digestion and elimination.
(In case you’re curious, pooping well-formed, easy-to-pass stools anywhere from three times a day to every other day is a sign of good elimination.)
Extra credit: Supplements that can help with indigestion, gas, and pooping.
Unfortunately, uncomfortable digestive symptoms sometimes still happen to people who do everything suggested in this article.
If you have mild indigestion, gas, or pooping problems—and can’t find any obvious culprits (or solutions)—supplements might be the extra nudge to get digestion and elimination back on track.
Here’s a list of common symptoms, and the supplements that can help:
| Symptom | Evidence-based supplement |
|---|---|
| Excessive gas / bloating | Specific digestive enzymes17 18 Select enzymes can help if you get symptoms after eating certain foods, such as alpha-galactosidase for beans and legumes, or lactase for dairy. Enteric-coated peppermint oil19 While peppermint oil can reduce pain, gas, and bloating, it can actually make acid reflux worse, if that’s a symptom you already experience. |
| Heartburn | Ginger, tea or capsules20 21 22 Ginger also helps with nausea. |
| Constipation | Magnesium citrate23 24 Magnesium is safe for long-term use, unlike most laxatives, which are habit-forming and aren’t good solutions for chronic constipation. |
| Diarrhea | Electrolytes & fluids25 Usually a sign of an acute infection, diarrhea is the body’s way of clearing out unwanted pathogens. For that reason, it’s often best to let it run its course. To reduce dehydration associated with diarrhea, hydrate with water, sports drinks, or over-the-counter rehydration solutions. |
If any of the above symptoms are severe or persist for more than a few days, contact your doctor.
For most people, the basics can really help.
You might be tempted to skip the above advice with a harrumphing:
“Blah blah blah, I KNOW this already! Isn’t there some more innovative, cutting edge protocol I can try??”
(Well, maybe. You could look into fecal transplantation. We’ll wait here while you decide that actually, you’ll try the basic diet and lifestyle changes after all.)
As many of our coaches and clients have experienced:
The challenge isn’t knowing what to do. It’s actually doing it, consistently.
Our advice?
Lean into consistency rather than novelty.
As in, “How can I slow down a little more at meals, or be a little more intentional about my veggie consumption” instead of “What’s the next trendy substance or protocol that promises to supercharge my microbiome?”
And if you need some motivation:
Changes in microbiome profiles can happen even within 24 hours of switching up your diet.26
So, wherever you’re starting from, when you add some basic practices, your gut bacteria may benefit within a short period of time.
(Nearly) instant gratification!
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build nutrition and lifestyle habits that improve their physical and mental health, bolster their immunity, help them better manage stress, and get sustainable results. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.